you're one step closer
Find Affordable Health Insurance With Plans Starting At $0/Month:
Call Now For Your 100% Free Quote
you're one step closer
Find
Affordable
Health Insurance
During the 2024 Special Enrollment Period
Call Now For Your 100% FREE Quote
OUR PARTNERS
GET COVERAGE FROM SOME OF THE TOP CARRIERS IN THE NATION
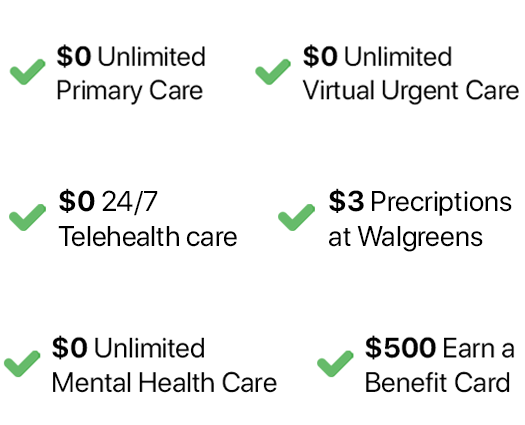
great PERKS
GET COVERAGE FROM SOME OF THE TOP CARRIERS IN THE NATION WITH BENEFITS SUCH AS:
OUR CORE VALUE

HOW IT WORKS
What is the Special Enrollment Period?
The Special Enrollment Period is a time outside the yearly Open Enrollment Period when you can sign up for health insurance. Depending on your Special Enrollment Period type, you may have 60 days before or 60 days following the event to enroll in a plan. You can enroll in Medicaid or the Children’s Health Insurance Program (CHIP) at any time.
The Special Enrollment Period for 2024 of the Health Insurance Marketplace runs from January 16, 2024, to October 31, 2024. If you missed the enrollment window, you may still be eligible to enroll for coverage.
If you’re unsure if you qualify for coverage under the Special Enrollment Period, we encourage you to contact an Insurance Advocate to see if there is anything we can do to help.


New Special Enrollment Period Changes for 2024!
New changes to the special enrollment period, grant year-round enrollment in ACA-compliant health insurance to some applicants if household income does not exceed 150% of the federal poverty level (FPL). Coverage will take effect the first of the following month.
There are no restrictions on how often this special enrollment period can be used or the type of health plan that can be chosen. A person with an eligible household income who is already enrolled in an exchange plan can utilize this SEP to switch plans, albeit the deductible and out-of-pocket expenditure for the year will be reset to $0 when the new plan begins.

